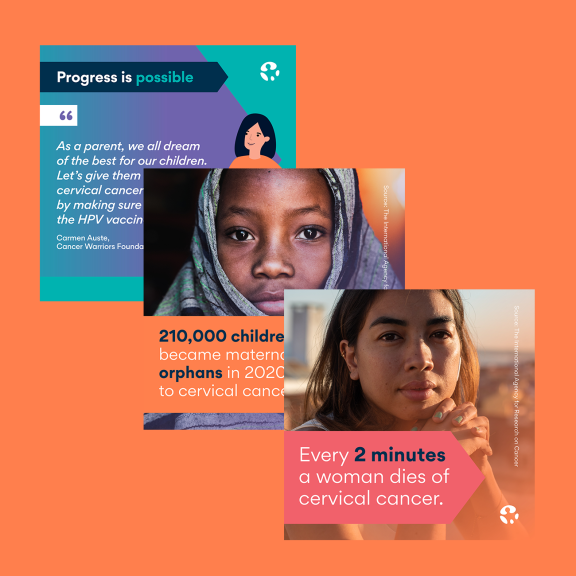
Spread
the word!
No woman should ever die from #cervicalcancer. Join us on 4 February and stand up for the elimination of cervical cancer. #WorldCancerDay #CloseTheCareGap worldcancerday.org/elimination
Aucune femme ne devrait mourir du #cancerducoldelutérus. Rejoignez-nous le 4 février pour agir en faveur de l'élimination du cancer du col de l'utérus. #JournéeMondialeContreLeCancer #PourDesSoinsPlusJustes
worldcancerday.org/elimination
Ninguna mujer debería morir de #CáncerDeCuelloUterino. Únase a nosotros el 4 de febrero y luche para acabar con el cáncer de cuello uterino. #DíaMundialContraElCáncer #PorUnosCuidadosMásJustos
worldcancerday.org/elimination